Supporting Telehealth During the COVID-19 Pandemic
KEY TAKEAWAYS
- Telehealth is playing a central role in the delivery of health care services during the COVID-19 pandemic.
- The Trump administration has taken steps to loosen regulations and has encouraged states to do the same, allowing telehealth to serve more patients and help mitigate the spread of the virus.
- Congress included provisions to expand telehealth in the CARES Act, including funding to help health care providers with broadband connectivity and telehealth devices, and supporting Telehealth Resource Centers nationwide.
The coronavirus pandemic has showcased how telehealth benefits public health by letting patients to connect with health care providers remotely. Considered a supplemental tool before the pandemic, it has become central to health care delivery, and there has been an increase in its use for conditions that would ordinarily be treated in-person. Telehealth has helped triage patients before they enter health care facilities, reducing unnecessary exposure to the virus. The Trump administration and Congress have taken steps to ensure telehealth’s reach expands and health care providers are paid appropriately for using the technology.
Supporting Telehealth during the COVID-19 Pandemic
Expanding telehealth’s reach
In an effort to reduce the risk of COVID-19 transmission, Secretary of Health and Human Services Alex Azar has waived federal licensing requirements, allowing patients in places hit hardest by the virus to get care from doctors practicing in other states. HHS also loosened related requirements of the Health Insurance Portability and Accountability Act to let patients communicate with their health care providers through audio and video communication apps such as Skype and Apple FaceTime.
The Centers for Medicare and Medicaid Services expanded access to telehealth services for Medicare beneficiaries, allowing them to stay in their home or assisted living facility to receive care during the public health emergency. This means patients have less need to travel to a health care facility and risk being exposed to, or spreading, the virus. Providers who might have been exposed to the virus can give some types of care remotely from their homes, helping to ease worker shortages during the pandemic. CMS added more than 80 services – including emergency room visits and nursing home screenings – to its list of approved care that can be provided through telehealth. The agency also is encouraging providers to evaluate Medicare patients via telephone, as some patients may not have the necessary technology for video screenings. Historically, the federal government has not reimbursed providers for telephone visits at the same rate as in-person consultations.
CMS further deregulated telehealth during the public health emergency. Through new blanket waivers and guidance related to the Coronavirus Aid, Relief, and Economic Security Act, the agency expanded the types of health care providers eligible to use telehealth. CMS authorized more providers – including counselors, physical and occupational therapists, and speech pathologists – to the list of providers who can deliver telehealth services to Medicare beneficiaries. These providers will still need to follow state laws and licensing requirements while practicing telehealth.
The CARES Act also took steps to promote and improve telehealth services in rural and underserved areas. The law reauthorized Health Resources and Services Administration grant programs that support the use of telehealth technologies for health care delivery, education, and information services. Through these programs, HRSA awarded $20 million to increase access and availability of telehealth services for vulnerable populations, including women and children with special health care needs, to prevent and respond to COVID-19.
Shifting care delivery
The CARES Act made changes to allow Medicare beneficiaries in hospice and with end-stage renal disease to get telehealth assessments. The law also authorized rural health clinics and federally qualified health centers to serve as “distant sites” for telehealth during the emergency, ensuring patients have more care options and clinics receive appropriate payment.
Congress provided $2oo million to the Federal Communications Commission to increase infrastructure for telehealth, making the technology accessible to patients who might not be able to get the services otherwise. HHS has awarded funding to organizations to help with this and to mitigate potential licensure and credentialing issues.
The law includes a provision to temporarily allow high-deductible health plans with health savings accounts to cover telehealth services before the beneficiary reaches his or her deductible. Depending on the plan, some patients may still be required to cover certain cost-sharing requirements. Throughout the pandemic, some insurers have expanded coverage and waived cost-sharing for telehealth services for the duration of the public health emergency.
Telehealth Visits Soar
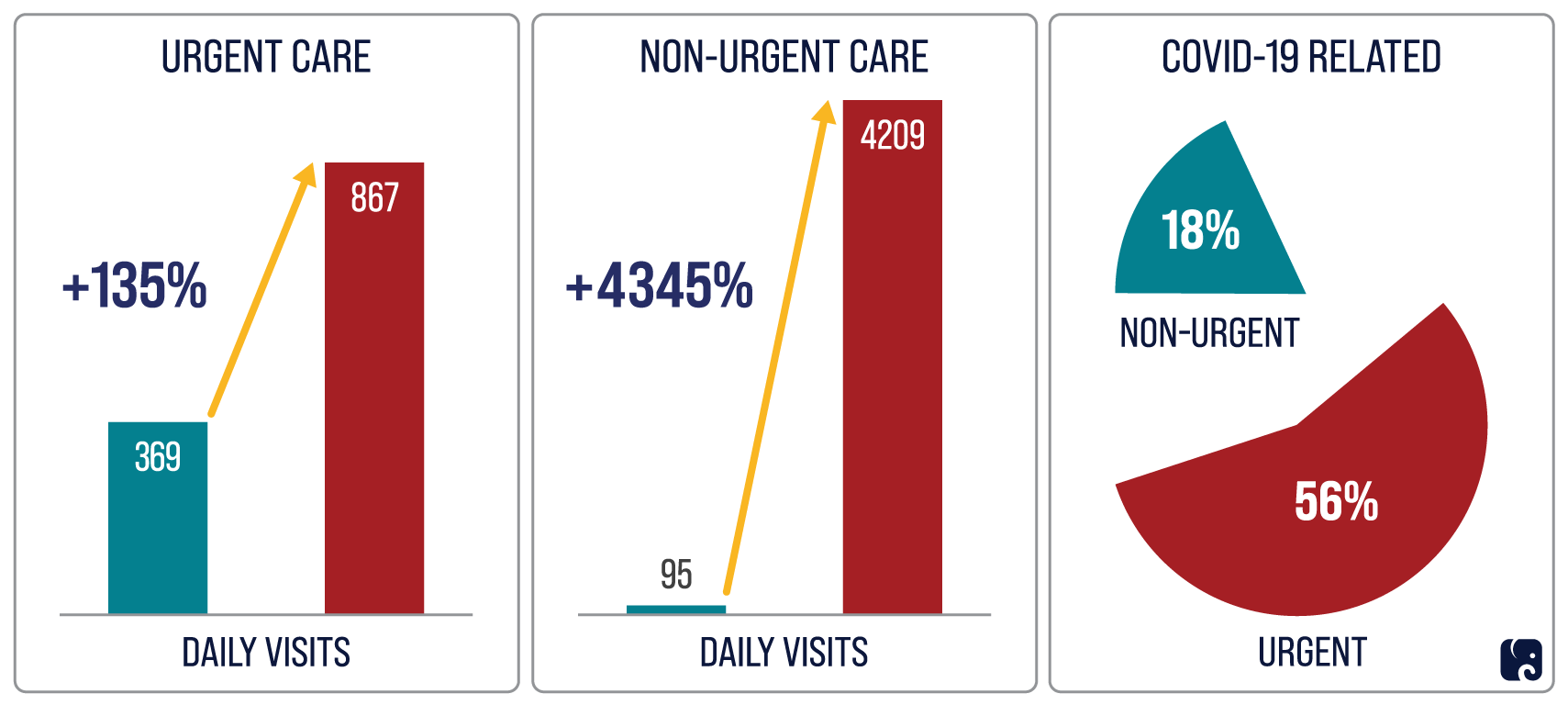
There is at least some data suggesting that patients and providers have adapted to using telehealth during the pandemic. According to a study evaluating telehealth use by NYU Langone Medical Center in New York, daily telehealth visits for urgent care visits increased by 135% from March 2 to April 14. Non-urgent care visits by telehealth increased by 4,345% during that period – from about 95 per day to more than 4,200. By mid-April, 56% of urgent visits were related to COVID-19, but only 18% of non-urgent visits were related to the disease. The study’s authors suspect that the COVID-19 pandemic may permanently increase the use of telehealth.
Next Article Previous Article
