Modernizing VA's Electronic Health Record System
KEY TAKEAWAYS
- The Department of Veterans Affairs manages one of the largest health care networks in the country, serving more than 9 million veterans at 1,255 locations throughout the U.S.
- The VA is in the midst of a 10 year, $16 billion modernization of its electronic health records system to improve interoperability with the Defense Department and private health care providers and to keep pace with advances in technology.
- On October 24, the VA reached a milestone with the deployment of the new system at a facility in Spokane, Washington; the VA plans to continue to roll out the new system in regional waves, finishing in 2028.
America has an obligation to care for those who have served our country in the military. Today, the Department of Veterans Affairs manages one of the largest health care delivery networks in the country, serving more than 9 million enrolled veterans at 1,255 health care facilities, including 170 medical centers and 1,074 outpatient sites.
The VA’s electronic health records system, known as VistA, has been essential to the department’s ability to deliver care for three decades, but it is outdated, costly, and difficult to maintain. The current system also does not work well with the systems used by the Department of Defense or most private health care providers.
In 2017, after years of failed efforts to modernize VistA or build a new EHR system, the VA decided to purchase the same commercial system selected in 2015 by DOD, which was also in the midst of a long-needed modernization. The transition is one of the most expensive and ambitious government IT modernization projects in history. It is scheduled to take 10 years and cost at least $16 billion.
the american heroes the va serves
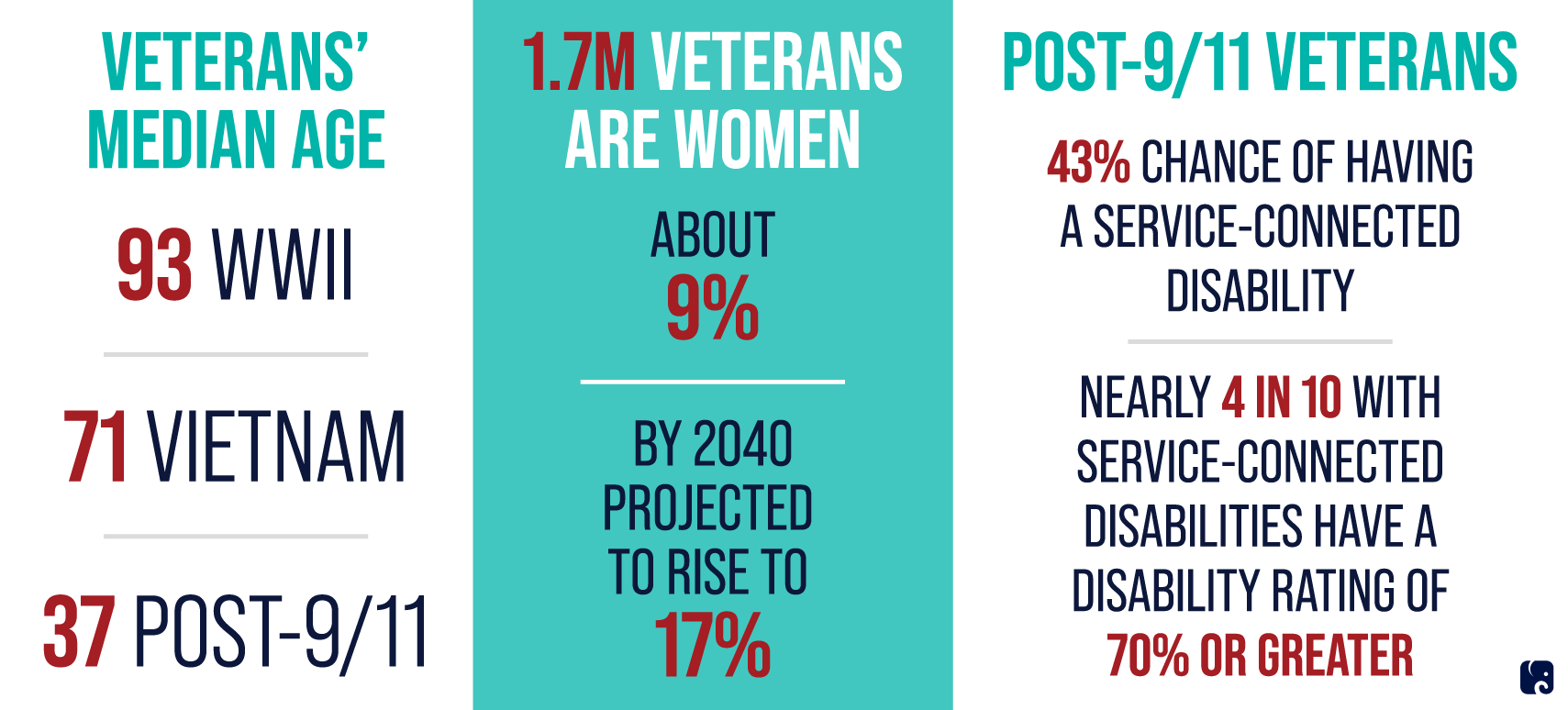
More than 41 million Americans have served in the U.S. armed forces over the nation’s history. There were 18 million living veterans as of 2018 − 7% of the U.S. population. Wars have affected the people who fight them differently, and as the demographics of the veteran population change over the years, the emphasis of the VA changes.
Of the 16 million Americans who served during World War II, there are fewer than 500,000 alive today, down from 5.7 million at the turn of the century. Most are at least 90 years old, with the health care needs that accompany very old age.
Vietnam-era veterans make up the largest cohort of veterans alive today, with 6.4 million who served from 1964 t0 1975. Many continue to deal with the effects of that conflict, some suffering from post-traumatic stress disorder, others from exposure to Agent Orange and other herbicides.
With the opening of combat roles to women in the 1990s, the number of female veterans has increased significantly. Between 1980 and 2018, the percentage of female veterans more than doubled, from 4% to 9%. Women make up about 15% of Gulf War-era veterans and 17% of all post-9/11 veterans.
Vets from Different Eras Have Different Health Care Needs
a troubled history of trying to modernize
The VistA system, which includes electronic health records as well as many other administrative and financial applications, has been in place since the early 1980s. Decades of modifications, some uniform across the country and others localized at individual medical centers, have created a hodgepodge of proprietary, commercial, and customized software in 130 slightly different versions of VistA. The VA refers to these different versions as “instances.”
VistA will be difficult to replace because of the wide range of functions it performs, some unrelated to health care, and the fact that VA built the system over decades to fit its unique processes. Making the transition to a commercial EHR system requires VA to conform to more standard health care delivery practices.
An additional obstacle to modernization is that VistA is programmed in an outdated computer language from the 1960s known as MUMPS. There are few software developers qualified to program in the language, and few modern systems use the language, creating interoperability challenges. These are common problems in modernizing “legacy” IT systems.
The VA has tried repeatedly over the past 20 years to modernize VistA and make it interoperable with DOD. In 2008 Congress mandated it, requiring DOD and VA establish fully interoperable EHR systems that would allow for sharing health care data across departments. In 2013, the VA launched yet another plan to modernize the system, dubbed “VistA Evolution.” The program expanded the use of the “Joint Legacy Viewer,” a tool that allowed VA medical personnel to view a read-only display of patient data from DOD and other health care providers. While an improvement, the JLV was a far cry from true interoperability.
The VA pursued elements of the VistA Evolution plan with mixed success over the next four years before, in June 2017, the department announced a significant shift. Rather than continue to pursue modernization of VistA, the department would procure the same commercial off-the-shelf EHR system that DOD was acquiring: Cerner Millennium.
rolling out the new system
The future of health care for service members and veterans will require closer integration between the VA, the Military Health System, and other health care providers. This is especially true since passage of the VA Mission Act, which allows veterans to use approved non-VA medical centers near them. Adopting a commercial EHR is essential to finally achieving a seamless, lifetime health record and true interoperability with private health care providers.
In May 2018, the VA awarded a contract to the Cerner Corporation to replace all 130 “instances” of VistA with a standard system to be implemented across the department. The project is the largest EHR implementation ever, and one of the most expensive and ambitious government IT modernization projects in history. It is currently scheduled to take 10 years and cost $16 billion. For fiscal year 2020, the program was appropriated about $1.5 billion. The final fiscal year 2021 appropriation is slated to exceed $2.6 billion. Funds and progress are tracked as a major IT investment on the Office of Management and Budget’s Federal IT Dashboard.
On October 24, the VA medical center in Spokane, Washington, became the first to begin using elements of the new system. The VA and Cerner reportedly plan to bring the facilities in Walla Walla, Washington, and Roseburg and White City, Oregon, online next, followed by others in Washington and Oregon. From there, the department expects to continue to roll out the new system in regional waves across the country through 2028.
Next Article Previous Article
