Senate Amendment to H.R. 1628 - Better Care Reconciliation Act
Noteworthy
Background: Leader McConnell released the second discussion draft of the Senate amendment to H.R. 1628, the Better Care Reconciliation Act of 2017, on July 13.
Floor Situation: Leader McConnell is expected to bring up the motion to proceed to H.R. 1628 next week.
Section-by-Section Summary
Title 1
Section 101 – Elimination of Limitation on Recapture of Excess Advance Payments of Premium Tax Credits
The bill repeals the dollar amount limits placed on subsidy repayment for people who received an excess advance premium tax credit, beginning in tax year 2018. Under Obamacare, if someone received too much, there are limits on what the government can collect.
Section 102 – Restrictions for the Premium Tax Credit
Beginning in 2020, the bill makes significant changes to the eligibility criteria for the premium tax credit. Under Obamacare, people with incomes between 100 percent and 400 percent of the federal poverty level are eligible for the credit. Under this bill, those with incomes from zero percent to 350 percent of FPL are eligible for the credit. The credit will begin to phase out at 300 percent of FPL.
The bill also adjusts how the premium tax credit is calculated (see chart below). It changes the income percentage that a recipient is required to pay before the credit kicks in and adjusts the required income percentage by age. This change would protect low-income people from having to pay a higher percentage of their income on premiums. In addition, the credit amount becomes more generous for younger adults and requires older adults at higher incomes to pay a greater share of their income on premiums before the credit kicks in to offset the cost of coverage.

The credit amount is benchmarked to the median premium of a plan with actuarial value of 58 percent in a geographic region, similar to a bronze or catastrophic plan. Previously, the credit amount was benchmarked to the second-lowest cost plan with an actuarial value of 70 percent, a silver plan, in a region. The bill also allows the credit to be applied to the purchase of a catastrophic health plan.
The aggregate growth of the premium tax credits will be slowed if the cost to the federal government reaches 0.4 percent of gross domestic product, compared to a higher threshold under current law, which is 0.504 percent of GDP.
The credit is only available to purchase coverage on the exchanges. It is only offered to people with qualifying incomes who are ineligible for coverage under a government program and not offered employer-sponsored insurance. The bill removes the affordability requirement for employer-sponsored insurance. To receive the credit, a person must be a citizen, national, or “qualified alien” and cannot be incarcerated.
The credits would also be “advanceable” – meaning they can go directly from the government to an insurer each month. The recipient would not have to wait until he files his taxes to receive advance payments of the credit. They would also be “refundable,” meaning he could collect the full credit even if he does not owe any income taxes.
Beginning in 2018, the bill modifies the definition of a “qualified health plan” to exclude plans that cover abortions other than to save the life of the mother or in the case of a pregnancy that is the result of rape or incest.
Section 103 – Modifications to Small Business Tax Credit
Excludes any health plan that covers elective abortion from being eligible for the small business tax credit and repeals the small business tax credit beginning in 2020.
Section 104 – Individual Mandate
Effectively repeals the individual mandate by lowering the penalty to $0 beginning in taxable year 2016.
Section 105 – Employer Mandate
Effectively repeals the employer mandate by lowering the penalty to $0 beginning in taxable year 2016.
Section 106 – State Stability and Innovation Fund
The bill creates two funds, for a total of $182 billion in federal dollars, to promote market stability and encourage state innovation over both the short-term and the long-term.
Short-term assistance to address coverage and access disruption and provide support for states:
The short-term fund allocates a total of $50 billion – $15 billion a year for calendar years 2018 and 2019 and $10 billion a year for 2020 and 2021.
The administrator of the Centers for Medicare and Medicaid Services would have wide latitude to use the money to fund arrangements with health insurance companies to address coverage and access disruption and respond to urgent health care needs. The funds appropriated will remain available until expended.
Not later than 30 days after enactment of this bill, the administrator will issue guidance to health insurance issuers regarding how to submit a notice of intent to participate in the program. Issuers will have to submit a notice of intent to participate for 2018 within 35 days of enactment. For 2019, 2020, and 2021, issuers will have to submit a notice to participate by March 31 of the previous year.
The administrator will determine how to distribute funds. One percent of the amount appropriated for this fund will be reserved for health insurance issuers in states where the cost of health insurance is at least 75 percent higher than the national average. Insurance issuers are not required to provide a funding match.
The funds may not be provided to any insurance plan that provides coverage of elective abortions.
Long-term state stability and innovation program:
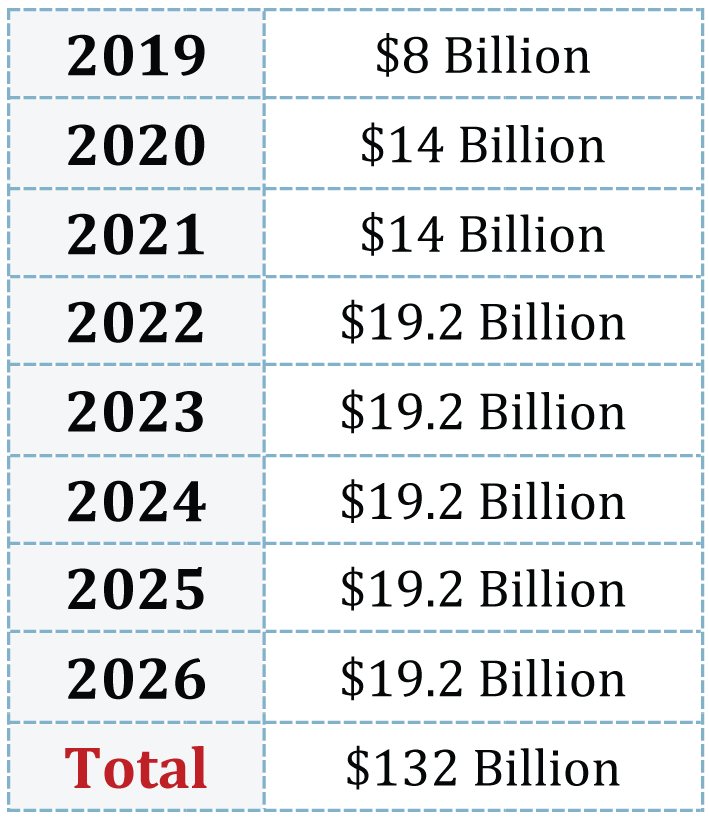
The long-term fund provides a total of $132 billion from 2019 to 2026 (see chart below).
The bill outlines four allowable uses for the funds:
-
To establish or maintain a program or mechanism to provide financial assistance – including by reducing premium costs – to help high-risk people who have or are projected to have a high rate of utilization of health services, as measured by cost;
-
To establish or maintain a program to enter into arrangements with health insurance issuers to help stabilize premiums and promote state health insurance market participation and choice in plans offered in the individual market;
-
To provide payments for health care providers for the provision of health care services;
-
To provide assistance to reduce out-of-pocket costs, such as copayments, coinsurance, and deductibles, of people enrolled in plans offered in the individual market.
Of these funds, the administrator shall ensure that at least $5 billion a year in years 2019, 2020, and 2021 is used for purpose two explained above. In addition, at least 1 percent of the amounts appropriated must be reserved for states where the cost of health insurance is at least 75 percent higher than the national average.
The funds are prohibited from going to the health insurance coverage of abortion services.
A state must submit an application for funds not later than March 31 for funds the following year. Funds are available for two years.
States apply for the funds and are approved for all subsequent years through 2026 unless the CMS administrator finds the state to be out of compliance.
In 2022, states would be required to start making contributions to the fund, beginning with a 7 percent match and increasing 7 percent each year until reaching a 35 percent contribution amount in 2026.
Section 107 – Better Care Reconciliation Implementation Fund
The Department of Health and Human Services is provided $500 million to implement the bill.
Section 108 – Repeal the Tax on Employee Health Insurance Premiums and Health Plan Benefits
Obamacare’s 40 percent excise tax on high-cost employer health plans, commonly referred to as the Cadillac tax, is delayed until 2026.
Section 109 – Repeal of Tax on Over-the-Counter Medications
Repeals the exclusion of over-the-counter medicines from the allowable uses of tax-advantaged health accounts, effective beginning in taxable year 2017.
Section 110 – Repeal of Tax on Health Savings Accounts
Repeals the tax increase for purchasing nonqualified medical expenses with tax-advantaged health accounts, effective for distributions made beginning in 2017. Obamacare raised the penalty from 10 percent to 20 percent for HSAs, this lowers it back down to 10 percent.
Section 111 – Repeal of Limitations on Contributions to Flexible Spending Accounts
Repeals the $2,500 limit on contributions to flexible spending accounts, effective beginning in plan year 2018.
Section 112 – Repeal of Tax on Prescription Medications
Repeals the tax on prescription drugs, effective calendar year 2018.
Section 113 – Repeal of Medical Device Excise Tax
Repeals the 2.3 percent excise tax on medical devices, effective for sales beginning in calendar year 2017.
Section 114 – Repeal of Health Insurance Tax
Repeals the health insurer tax, effective calendar year 2017.
Section 115 – Repeal of Elimination of Deduction for Expenses Allocable to Medicare Part D Subsidy
Repeals the elimination of the employer deduction for retiree prescription drug coverage, effective beginning in taxable year 2017.
Section 116 – Repeal of Chronic Care Tax
Repeals the increase in the amount of income that must be spent on medical expenses before a deduction is allowed, lowering it from Obamacare’s 10 percent to 7.5 percent, effective beginning in taxable year 2017.
Section 117 – Repeal of Tanning Tax
Repeals the 10 percent indoor tanning tax, effective September 30, 2017.
Section 118 – Purchase of Insurance from Health Savings Account
Allows qualified medical expenses to include amounts paid for an account holder’s children who are under the age of 27. Also allows HSA funds to be used to pay premiums for a high deductible health plan to the extent the premium exceeds: any tax deduction allowable; any amount excludable from income tax; and any tax credit amount allowed. The amendments under this section would become effective in 2018.
Section 119 – Maximum Contribution Limit to HSA Increased to Amount of Deductible and Out-of-Pocket Limitation
The maximum contribution for health savings accounts is nearly doubled. It is increased to the sum of the annual deductible plus the maximum out-of-pocket expenses permitted under a high deductible health plan. Effective beginning in taxable year 2018.
Section 120 – Allow Both Spouses to Make Catch-Up Contributions to the Same Health Savings Account
Both spouses can make catch-up contributions to the same health savings account, beginning in taxable year 2018.
Section 121 – Special Rule for Certain Medical Expenses Incurred Before Establishment of Health Savings Account
HSA funds may be used to pay for qualified medical expenses incurred during the 60 day period after enrollment in a high deductible health plan and before the account is established, beginning for coverage that begins in 2018.
Section 122 – Exclusion from HSAs of High Deductible Health Plans Including Coverage for Abortion
HSA funds could not be used to pay for a high-deductible health plan that covers abortions except if necessary to save the life of the mother or if the pregnancy is the result of rape or incest.
Section 123 – Federal Payments to States
Prohibits for one year federal payments – including Medicaid, the Children’s Health Insurance Program, Maternal and Child Health Services Block Grants, and Social Services Block Grants to states – from going to certain non-profit, family planning entities that receive more than $350 million a year in Medicaid funding and provide abortion services.
Section 124 – Repeal of Medicaid Provisions
The bill prohibits hospitals that participate in Medicaid from making presumptive-eligibility determinations, intended to give people access to benefits before their application is approved, effective January 1, 2020.
It repeals the increased federal match rate for the Community First Choice option, effective January 1, 2020.
Section 125 – Repeal of Medicaid Expansion
The bill repeals the state option to extend coverage to non-elderly adults above 133 percent of FPL after December 31, 2017.
Beginning in 2021, the Obamacare enhanced payment rate for all expansion-population enrollees will begin to decline 5 percentage points a year until 2024. In 2024, a state will receive its normal federal matching payment for the expansion population.
All states will be allowed to cover people earning less than 133 percent of the federal poverty level, but will have their payment decline over time until 2024, when the payment will be the state’s normal FMAP.
States that did not expand Medicaid prior to March 1, 2017, are ineligible to receive the Obamacare enhanced matching rate.
Repeals the essential health benefits requirement for Medicaid beneficiaries beginning after December 31, 2019.
Section 126 – Restoring Fairness in DSH Allotments
Obamacare reduced disproportionate share hospital payments – intended to cover uncompensated care – to all states. Beginning in 2018, Obamacare’s cuts to Medicaid DSH payments will be no longer be in effect for states that did not expand Medicaid. States that did expand Medicaid will have their DSH payments fully restored in 2020.
In addition, non-expansion states that have a per-capita DSH payment that is below the national average will have their payment amount raised to the national average beginning in 2020 and ending in the second quarter of 2024.
The amount will be based on the number of uninsured people in the state in the year with the most recent data available.
Section 127 – Reducing State Medicaid Costs
Limits retroactive enrollment in Medicaid to the month in which the applicant applied, beginning October 1, 2017.
Section 128 – Safety-Net Funding for Non-expansion States
Provides $10 billion over fiscal years 2018-2022 to non-expansion states to increase payments to Medicaid providers. Each state’s allotment of the $2 billion per year will be based on the number of residents below 133 percent of the poverty line in 2015, relative to the total number of people below this amount in all other non-expansion states. If a state expands Medicaid, it is no longer eligible for this safety-net funding the following years.
Section 129 – Eligibility Redeterminations
Allows states to increase the frequency of Medicaid eligibility redeterminations to every six months and increases administrative funding for states that opt for more frequent redeterminations.
Section 130 – Optional Work Requirement for Non-disabled, Non-elderly, Non-pregnant People
Beginning October 1, 2017, states may elect to impose work requirements on their able-bodied, non-elderly, adult populations. The law provides enhanced administrative funding for states that take this option.
Section 131 – Provider Taxes
Phases down the allowable Medicaid provider tax threshold from 6 percent to 5 percent. The phase down is a 0.2 percent reduction each year from fiscal year 2021 to fiscal year 2025.
Section 132 – Per-Capita Allotment for Medical Assistance
Starting in fiscal year 2020, states will receive a capped amount of money per Medicaid enrollee, based on the category of eligibility into which the enrollee falls. There are five Medicaid categories: elderly; blind and disabled; children; non-expansion adults; and expansion adults. The initial payment amount will be based on a state’s per capita base period calculation. For this calculation, a state may pick any eight consecutive quarters from quarter one of fiscal year 2014 to quarter three of fiscal year 2017. The sum of applicable expenditures of those eight quarters is divided by two to create an artificial four fiscal quarter period to use as the per capita base period.
States that expanded their Medicaid programs later than the fourth quarter of 2015 but before the fourth quarter of 2016 may select a period shorter than eight consecutive quarters, but not less than four.
Funding for the elderly and the blind and disabled will be indexed to annual increases in the medical care component of the urban consumer price index – CPI-U – inflation rate plus 1 percent from 2020-2025. Funding for all other categories will be indexed to increases in the medical care component of the urban CPI from 2020-2025. For fiscal years 2025 and 2026, all populations’ cap amount will be indexed to increases in the CPI-U. If a state’s spending exceeds the cap, its federal Medicaid funding will be reduced the following year.
Non-DSH supplemental payments will be included in the caps. Certain populations, such as blind and disabled children, Children’s Health Insurance Program and Indian Health Service enrollees, breast and cervical cancer services eligible enrollees, and partial-benefit enrollees, would be exempt from the caps.
In addition, beginning on January 1, 2020, and ending on December 31, 2024, if a state experienced a public health emergency as declared by the secretary of HHS, the state’s Medicaid spending would be excluded from the caps. The total amount of funds excluded from the caps cannot exceed $5 billion.
Beginning in 2020, a state’s target per capita medical assistance spending for each enrollee category will be adjusted if the state’s spending in that category in the previous year departed from the national average by 25 percent or more. If a state’s spending was less than 25 percent below the national average, the secretary of health and human services could increase the payment. If it was greater than 25 percent of the national average, the secretary could decrease the payment. These adjustments would not apply to low-density states.
The secretary shall create a new demonstration project to provide and improve the quality of home and community-based services beginning January 1, 2020, and ending on December 31, 2023.
Section 133 – Flexible Block Grant Option for States
Beginning in fiscal year 2020, states may choose to receive a block grant for providing health care for their non-elderly, non-disabled adult population – expansion and non-expansion – rather than the per capita allotment.
Funding for the block grant would be determined using the same base year calculation as the state’s per capita allotment. The grant amount will be indexed to the CPI-U inflation rate. Unspent funds may be rolled over for the subsequent year.
The block grant lasts for five years, with the option to continue every five years after notification to CMS.
States that elect to use the block grant option have the ability to determine scope, duration, and amount of all mandatory benefits. At a state’s discretion, optional benefits can also be included.
The secretary may make additional payments to states with a block grant in the case of a public health emergency.
Section 134 – Medicaid and CHIP Quality Performance Bonus Payments
There will be $8 billion available beginning in fiscal year 2023 through fiscal year 2026, for a state that spends below the per capita allotment and submits the required paperwork to HHS. Because states may not keep what they save if they spend below the cap, this fund provides some money to reward the most efficient states.
Section 135 – Grandfathering Certain Medicaid Waivers
States that are operating “managed care waivers” that have not substantially changed for 10 years or more may continue their waiver in perpetuity without needing re-approval. If a state does seek to modify an existing waiver, it is deemed approved unless the secretary responds within 90 days.
Section 136 – Coordination with States
Created a requirement for the secretary of HHS to engage in additional policy consultation with states and additional Medicaid rulemaking procedures, effective for rules finalized on or after January 1, 2018.
Section 137 – Optional Assistance for Certain Inpatient Psychiatric Services
States have the option to lift the Medicaid exclusion for institutions for mental disease from facilities based on beds in a facility, and instead can cover inpatient psychiatric services for substance use disorders and mental health for up to 30 consecutive days, but no more than 90 days per year.
States that utilize this option will be required to maintain: 1) the number of licensed beds; 2) the annual level of state spending for a: inpatient services and b: active psychiatric care and treatment. States would receive a 50 percent FMAP for Medicaid enrollees over age 21 and under 65. Effective October 1, 2018.
Section 138 – Enhanced FMAP for Medical Assistance to Eligible Indians
The bill changes the federal matching assistance percentage to 100 percent for services provided to a member of an Indian tribe and eligible for assistance under a Medicaid state plan.
Section 139 – Small Business Health Plans
Establishes a new type of health plan, Small Business Health Plans, to be treated as group health plans. A sponsor of SBHPs must offer fully insured plans, be established for purposes other than offering health insurance, and obtain certification from the secretary of the Department of Labor.
Title II
Section 201 – The Prevention and Public Health Fund
Rescinds all funds for the Prevention and Public Health Fund beginning in fiscal year 2019.
Section 202 – Support for State Response to Opioid and Substance Abuse Crisis
Appropriates $4.972 billion in each fiscal year from 2018 through 2026 ($45 billion total) for HHS to provide grants to states to support treatment and recovery services for people with mental and substance use disorders, which many states may use to address the opioid crisis. In addition, $50.4 million each fiscal year from 2018-2022 for research on addiction and pain related to the substance abuse crisis. The funds remain available until expended.
Section 203 – Community Health Center Program
Increases funding for community health centers by $422 million in fiscal year 2017.
Section 204 – Change in Permissible Age Variation in Health Insurance Premium Rates
Changes Obamacare’s age-rating restriction from 3:1 to 5:1, or a ratio determined by states. This means an older person would not be charged a premium more than 5 times higher than a younger person.
Section 205 – Medical Loss Ratio Determined by State
Changes Obamacare’s medical loss ratio for individual, small group, and large group health plans to a ratio determined by states.
Section 206 – Stabilizing the Individual Insurance Markets
Starting in 2019, consumers who have a 63 day gap in creditable coverage in the prior year will be subject to a six-month waiting period before coverage begins. Consumers will not have to pay premiums during this six-month period.
Membership in a health care sharing ministry is included in the definition of creditable coverage.
Section 207 – Waivers for State Innovation
The bill makes substantial changes to Obamacare’s Section 1332 waiver, which allows states to receive funding to create their own health insurance reforms. These changes would make it both faster and easier to obtain a funding and a waiver, giving states the potential for significant flexibility.
Under current law, a state may waive the following:
-
Definition of qualified health plan, including requirements related to essential health benefits, actuarial value, and limits on cost-sharing
-
Establishment of health insurance exchanges
-
Cost-sharing subsidies
-
Premium tax credits
-
Individual and employer mandates
However, a state may only obtain a waiver if the secretary determines that the state’s plan meets the following requirements:
-
Provides coverage at least as comprehensive as under Obamacare, which is to be certified by the office of the CMS actuary;
-
Provides coverage and cost-sharing at least as affordable as under Obamacare;
-
Provides coverage to at least as many people as under Obamacare; and
-
Will not increase the federal deficit
The bill amends the existing waiver to strike these requirements, which have been a barrier to states receiving funding. The Senate language requires 1332 waiver applications to include a description of how the state plan will replace the requirements being waived, provide alternative means for increasing coverage, lower premiums, or provide consumers the freedom to purchase the health insurance of their choice. The secretary shall approve a state’s request unless the plan would increase the federal deficit or is missing a required element of the application.
In addition, the bill allows the new stability funding to be used as pass-through funding through the waiver.
The bill provides $2 billion in grants to assist states in the application of Section 1332 waivers.
Section 208 – Allowing All Individuals Purchasing Health Insurance in the Individual Market the Option to Purchase a Lower Premium Catastrophic Plan
Obamacare barred people over the age of 30 from purchasing catastrophic coverage and barred eligible individuals from using a tax credit to buy such coverage. This provision allows anyone to buy a catastrophic plan regardless of age, and allows those eligible for tax credits to put their credit toward a catastrophic plan.
Section 209 – Application of Enforcement Penalties
Obamacare requires insurers to separate the cost of abortion coverage from the rest of the medical coverage and charge a separate fee for it. Some insurers have violated this requirement in the past. This provision establishes a penalty that can be enforced by the secretary for violations of Obamacare’s abortion funding segregation requirements. The penalty can still be enforced even if a state receives a 1332 State Innovation Waiver.
Section 210 – Funding for Cost-Sharing Payments and Section 211 – Repeal of Cost-Sharing Subsidy Program
People between 100 percent and 250 percent of the federal poverty level get cost-sharing reduction subsidies to reduce their out-of-pocket expenses. These are in addition to any premium tax credit they receive. A person must be enrolled in a silver plan to receive CSR payments. This bill provides an appropriation for CSRs for this year through 2019. Beginning in 2020, CSRs are repealed.
TITLE III
Section 301 – Establishing Federal Funding for Individual Market Plans
Out of the funds appropriated for the Stability Fund, $70 billion for calendar years 2020-2026 shall be used to establish a fund for the purpose of making payments to health insurance issuers that offer plans in a rating area off of the exchange that are not compliant with many of Obamacare’s federal insurance regulations. In order to offer noncompliant plans in that rating area, the health insurer would be required to offer at least one gold, one silver, and one benchmark Obamacare-compliant plan on the exchange in that rating area. Noncompliant plans would still be subject to state insurance regulation.
The Stability Fund money would be used by HHS to make payments to these issuers to offset the cost of high-risk individuals that purchase Obamacare-compliant plans on the exchanges in a given rating area.
The noncompliant plans would not be eligible for premium tax credits, but eligible individuals could use their health savings accounts to pay for premiums, subject to Hyde protections. Coverage in a noncompliant plan would not be considered creditable coverage, but would remain subject to Obamacare’s guaranteed renewability regulation. Thus, if an individual wanted to switch from a noncompliant plan to a compliant plan they would subject to the six month waiting period created under this bill.
Regulations of Obamacare that could be waived include:
-
Actuarial value
-
Essential health benefits
-
Requirements related to cost-sharing
-
Community rating
-
Guaranteed issue
-
Prohibition of preexisting condition exclusions
-
Prohibition of discrimination based on health status
-
Prohibition of waiting periods for group plans
-
Coverage of preventative health services without cost-sharing
-
Medical loss ratio
Regulations of Obamacare that could not be waived include:
-
Coverage of children up to age 26 on parents’ plan
-
Guaranteed renewability
-
Single risk pool requirement for an issuer offering on and off exchanges
-
Lifetime and annual limits
-
Federal rate review
-
Prohibition on rescissions
Administration Position
The administration has not taken a position on this bill at this time.
Cost
The Congressional Budget Office is expected to release a cost estimate of Titles I and II early next week.
