Telehealth Provisions Extended in the Omnibus
KEY TAKEAWAYS
- In 2020, Congress temporarily expanded Medicare patients’ access to telehealth services in response to the COVID-19 pandemic.
- Recognizing the value and increased use of telehealth, the fiscal year 2022 appropriations legislation kept several of these flexibilities in place.
- Telehealth use skyrocketed during the pandemic because of the increased flexibility, with behavioral health services seeing the largest increases.
Responding to the challenge of delivering routine care to patients during the COVID-19 pandemic, Congress temporarily expanded access to telehealth services for people on Medicare. Once health care providers were given this flexibility, telemedicine use grew rapidly, even while other visits by patients declined. The 2022 appropriations legislation that Congress passed earlier this month extended several telehealth flexibilities.
Telehealth Flexibility Led to Increased Use
Telehealth Use rose During the Pandemic
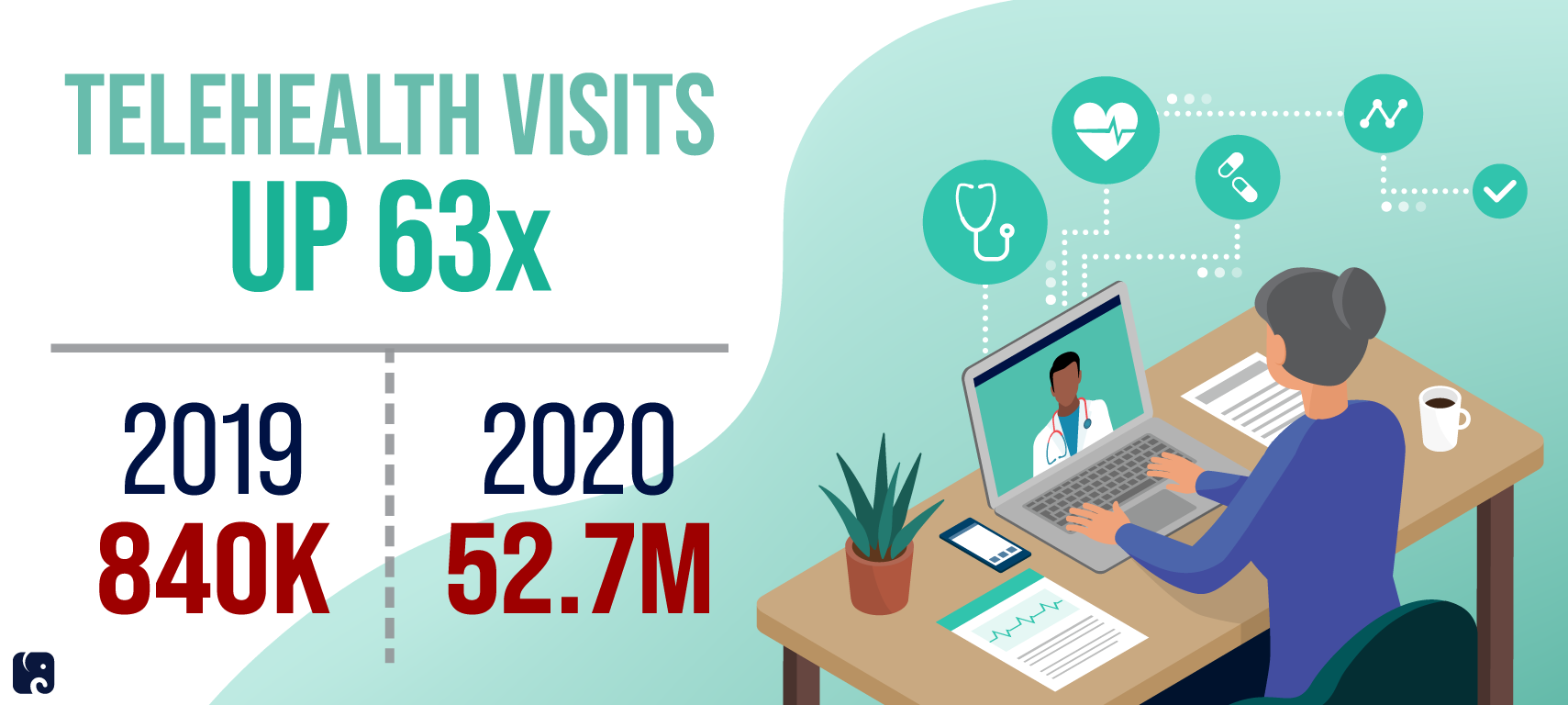
Prior to the pandemic, Medicare generally paid doctors and other health care providers only for visits in person. Coverage of telehealth was largely limited to a subset of services delivered via two-way audio-visual telecommunications to patients at designated sites in certain rural areas. Thanks to new flexibilities and waivers authorized by Congress and implemented by the Department of Health and Human Services in the early stages of the COVID-19 pandemic, telehealth use surged, particularly among older people. According to a report issued by HHS last December, Medicare beneficiaries had approximately 840,000 telehealth visits in 2019. In 2020, the number grew to nearly 52.7 million visits, a 63-fold increase. In-person services covered by Medicare Part B fell 16.1% in 2020, but expanded use of telehealth offset a sizable portion of this decline. They accounted for 5.3% of Part B visits that year, versus less than 1% a year earlier. The majority of these virtual visits occurred in patients’ homes, an option not available to most Medicare patients prior to the pandemic public health emergency.
While a range of primary care and specialty telehealth services saw substantial growth, the telehealth option proved particularly useful for beneficiaries seeking behavioral health care. According to HHS, “Visits to behavioral health specialists showed the largest increase in telehealth in 2020.” The agency found that 38.1% of all visits for behavioral health were conducted through telehealth that year, with roughly 70% of behavioral health telephone visits eligible for Medicare reimbursement. Mental health challenges and substance use increased dramatically during the pandemic, and behavioral health services are well-suited to telehealth.
Telehealth visits of all types peaked in the early months of the pandemic and then dropped off toward the end of 2020, as places began removing pandemic restrictions and doctors began seeing more patients in person. HHS says that telehealth use for behavioral health services, however, remained high at the end of the year.
extending telehealth provisions
The omnibus FY 2023 spending bill extended temporary provisions for telehealth services under Medicare beyond the COVID-19 public health emergency. Under that legislation, many of the core waiver policies currently tied to the pandemic will remain in place for at least 151 days beyond the end of the emergency period. This is intended to provide predictability for providers and patients, and to give more time for further evaluation. During that time:
-
Medicare beneficiaries can continue to receive covered telehealth services from any location, including their home.
-
Federally qualified health centers and rural health clinics can continue to deliver telehealth services, expanding access to care for underserved and rural communities.
-
Physical therapists, occupational therapists, audiologists, and other providers not eligible to deliver Medicare-covered telehealth services prior to the pandemic can continue to do so.
-
The in-person visit restrictions for mental health services, as passed by Congress and implemented through regulation, will continue to be delayed, eliminating potential access barriers for these services.
-
Medicare will continue to reimburse for audio-only appointments. This has helped rural patients with limited broadband connections and people who do not have, or cannot use, internet or video technology.
-
Qualified hospice providers can continue using telehealth technologies in order to fulfill the mandatory hospice face-to-face recertification requirement.
Congress is also requiring the Medicare Payment Advisory Commission and HHS to study and report on telehealth use during and after the public health emergency, as well as to recommend reforms. The department must consider ways to prevent telehealth fraud and abuse and to provide specific recommendations to increase telehealth use.
Outside of these permanent flexibilities and certain targeted updates advanced by HHS through regulation, however, the vast majority of waivers authorized by the CARES Act and other pandemic relief bills will expire at the end of the pandemic health emergency. Without congressional actions like the provisions included in the FY 2023 omnibus spending bill, this could create the risk of a telehealth access cliff at some point.
Next Article Previous Article
