Medicaid Home and Community-based Services
KEY TAKEAWAYS
- Democrats are trying to expand Medicaid and increase spending by $400 billion to advance their liberal wish list, disguising it as an expansion of home and community-based health care services.
- Their plan does not address the underlying challenges facing the Medicaid program, and it goes well beyond the program’s scope by providing mandates on states for non-health care benefits.
For decades there has been bipartisan support for providing home and community-based health care services. These services allow patients to get care in more comfortable or convenient settings of their choosing, rather than at institutions. States have been free to determine the benefits that worked best for their people. Democrats, as part of their reckless tax and spending spree, are seeking to harm the way these services are provided by conditioning new funds on changes that promote their liberal policy agenda.
$400B Medicaid Expansion Proposal
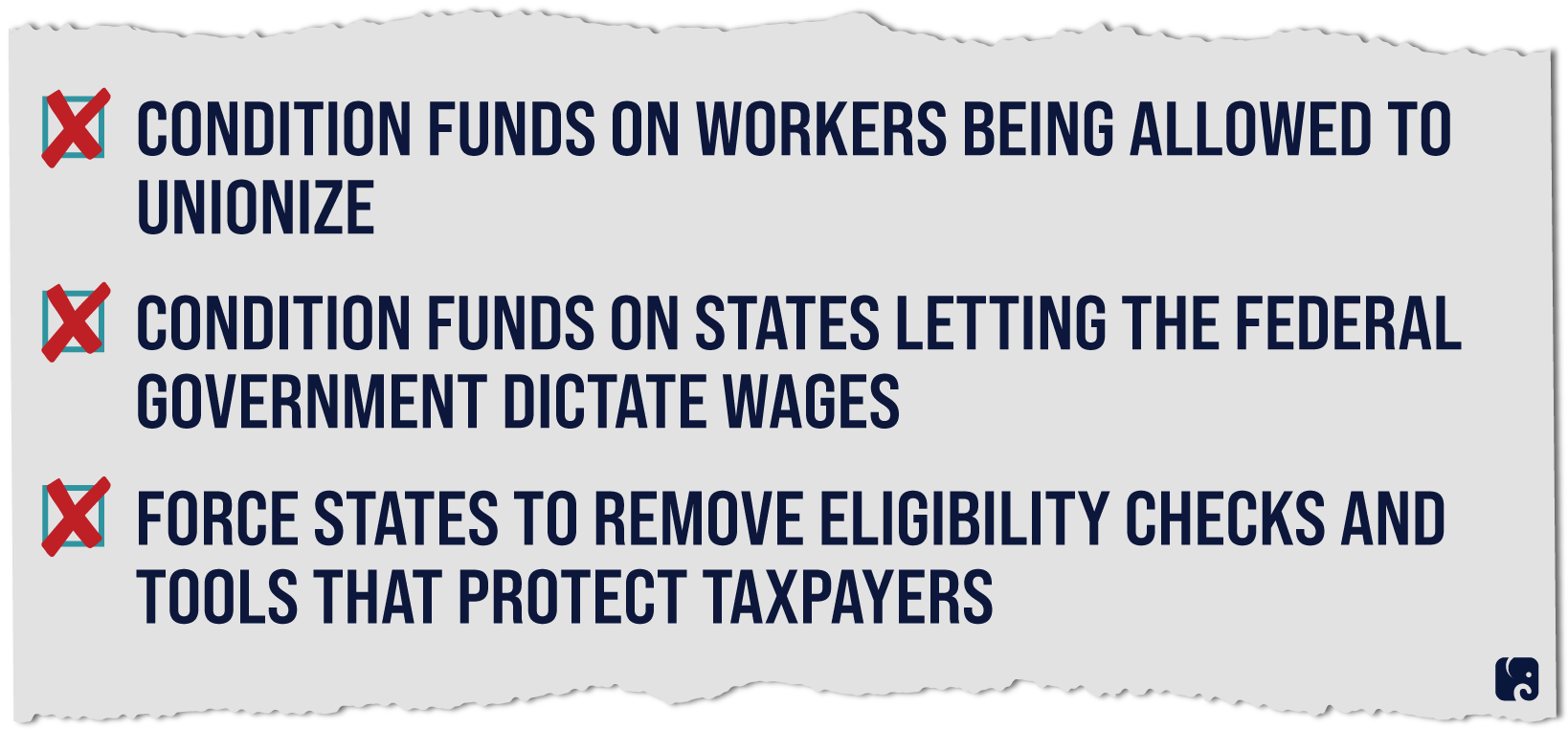
The federal government supports home and community-based services through Medicaid. President Biden is pushing for $400 billion in increased spending on these services, with requirements that states allow the federal government to dictate wages and that home health workers be allowed to unionize as a condition of receiving the additional money. States would be required to remove eligibility checks and other program integrity tools, which are intended to detect and combat fraud and misuse of taxpayer dollars. So in order to get the new money, states must surrender control of their programs.
the basics of hcbs
Medicaid is a joint federal and state program that delivers medical care and long-term services and supports to qualifying poor people, including children, pregnant women, people with disabilities, and senior citizens. Federal law requires states to provide certain health benefits through Medicaid, and it leaves to the state which, if any, optional benefits to cover. States and the federal government share the costs of providing Medicaid services.
States are required to cover nursing home services and limited home health services for eligible beneficiaries. These home health services include nursing, health aides, or medical supplies and equipment. States can choose to offer HCBS for beneficiaries who choose not to reside in nursing facilities, and adult day services, personal care services, and home-delivered meals. These services have allowed millions of Americans to stay in their homes rather than in institutions and given them more choice, autonomy, and self-directed care.
Every state currently offers Medicaid HCBS to some extent. The services are widely bipartisan, and states have made progress over the last decade in offering more services through HCBS. States set the range of benefits, eligibility thresholds, and benefit packages. Typically states do this through HCBS waivers, which allow them to target benefits to specific groups and set thresholds for the number of people receiving services. For example, states can create waiver services for adult day health, home health aides, and case management. They can target the services to specific groups, such as people with physical or developmental disabilities under the age of 65. Medicaid waivers give states the opportunity to experiment with innovative ways of providing care. Waivers under Section 1915(c) and Section 1115 of the Social Security Act are often used by states to provide HCBS and allow them to determine the number of people served.
What Democrats Are Proposing
In fiscal year 2019, Medicaid expenditures totaled $627 billion, and the federal share was $405 billion, nearly two-thirds of total. While less expensive than traditional nursing facilities, HCBS are an increasingly costly component of total Medicaid spending − a projected $114 billion this fiscal year. As the population ages, states expect to spend a larger share of their total Medicaid spending on long-term care, particularly HCBS.
Democrats have been trying to force states to move to a one-size-fits-all approach. The $2 trillion “COVID-19” bailout Democrats pushed through Congress in March encouraged states to devote more Medicaid spending to HCBS by increasing the federal matching rate for these services. The Congressional Budget Office estimates the law will increase Medicaid HCBS spending by another $12.6 billion in 2021 and 2022.
Now President Biden is pushing for his allies in Congress to force through another $400 billion to remove state flexibilities essential to providing better care. As a condition of receiving enhanced federal match for these Medicaid services, states would be required to expand Medicaid enrollment through the use of presumptive eligibility, which allows providers to be reimbursed for providing care to patients who may be eligible for Medicaid but are not yet enrolled. Some states have chosen to determine eligibility of enrollees more frequently to ensure those who are ineligible are removed from Medicaid. This helps ensure ineligible people don’t crowd out access for those who the program is intended to assist. States should be checking eligibility determinations more, not less. Adding a presumptive eligibility requirement removes states’ ability to safeguard against improper enrollment. According to the Kaiser Family Foundation, around 600,000 Americans with disabilities were on waiting lists for Medicaid services in 2018. Making it more difficult to remove ineligible people from the program will not help reduce the size of those wait lists.
In addition to dictating how states safeguard the integrity of their programs and taxpayer dollars, Democrats are pushing additional federal mandates. They would allow the federal government to set wages for the HCBS workers and would also require that the workers be allowed to join or form unions. Both of these would be federal requirements in order for states to get any of the new money.
Today, states can take many factors into account when determining how their programs work, including eligibility, financing, and benefit design. Democrats’ twin mandates would raise the cost of care for state Medicaid programs and limit the programs’ flexibility. They would also harm older Americans who do not qualify for Medicaid and who will likely pay more for these kinds of services.
The federal government is a partner with states in paying for Medicaid services. There is a role for Washington to help make the system more efficient, to improve the quality of benefits, and to make the system more patient-centered. The one-size-fits-all proposals made by Democrats include none of those reforms. Any steps by Congress should leave states to determine the best way to run their programs, free from unnecessary and potentially harmful federal mandates.
Next Article Previous Article
