Access to Mental Health Care
KEY TAKEAWAYS
- Last year, one in five American adults had a diagnosable mental illness, though only 43% got care.
- Many people who do seek care go to an emergency room, which may not be equipped to help them continue treatment.
- Certified community behavioral health clinics are one way the federal government is attempting to more appropriately coordinate mental health care.
According to the Substance Abuse and Mental Health Services Administration, more than 47 million American adults had a diagnosable mental, behavioral, or emotional disorder of some type last year. Only about 43% of them received mental health care during the year. Millions of people are not getting the care they should from an appropriate provider.

where people turn for help
When people who are having mental health problems do seek treatment, there are a wide variety of places they may go, some better suited than others to their specific needs. Patients might go to a hospital or outpatient clinic where they have access to staff psychiatrists, psychologists, addiction specialists, and trained nurses. Others end up getting treatment in an emergency room or being directed into the system by the police.
The rate of ER visits for mental health and substance use disorders increased by 44% between 2006 and 2014, the Agency for Healthcare Research and Quality has reported. Those patients’ need for treatment usually continues after they are sent home, but there is frequently no appropriate place to help coordinate their mental and behavioral health care. Without proper care, these patients are at further risk for homelessness and additional problems with the criminal justice system.
Making the problem worse, the Department of Health and Human Services says that there are more than 4,600 facilities across the country that have a shortage of mental health care providers.
Community-focused care
Since the late 1960s, there has been a trend to deinstitutionalize care, closing large facilities and encouraging mental health care services to be focused at the community level. Many of the proposed community health centers were never built, and communities were unprepared to address the needs of their residents. Consequently, many people with mental illnesses were shifted to jails and homeless shelters.
Signs of Progress at Certified Community Behavioral Health Clinics
In the 2014 Excellence in Mental Health Act, Congress tried a different approach to help provide mental and behavioral health care services at the community level. The law established a demonstration program for certified community behavioral health clinics to deliver comprehensive health care services with a focus on mental health care and addiction treatment. These clinics are funded through Medicaid and have reimbursement rates based on their expected costs of providing care.
Eight states are part of the demonstration: Minnesota, Missouri, Nevada, New Jersey, New York, Oklahoma, Oregon, and Pennsylvania. The clinics care for patients regardless of where they live or their ability to pay. Patients get access to 24-hour crisis management services and to preventive screenings to determine appropriate care coordination with other providers, such as emergency departments and veterans services. Patients also have access to primary care assessment and monitoring, caregiver support, and intervention and stabilization services.
CCBHCs can provide multiple services for a patient in one setting, rather than forcing someone to navigate a complex health care system. As a result, patients may be more likely to stick with their treatment. Demonstration funds are being used to address provider shortages, with an average of 46 new staff per CCBHC, including additional psychiatrists specializing in addiction or the treatment of children. One survey of clinics certified under the program found that 90% of them had been able to increase their patient loads, by an average of 25%.
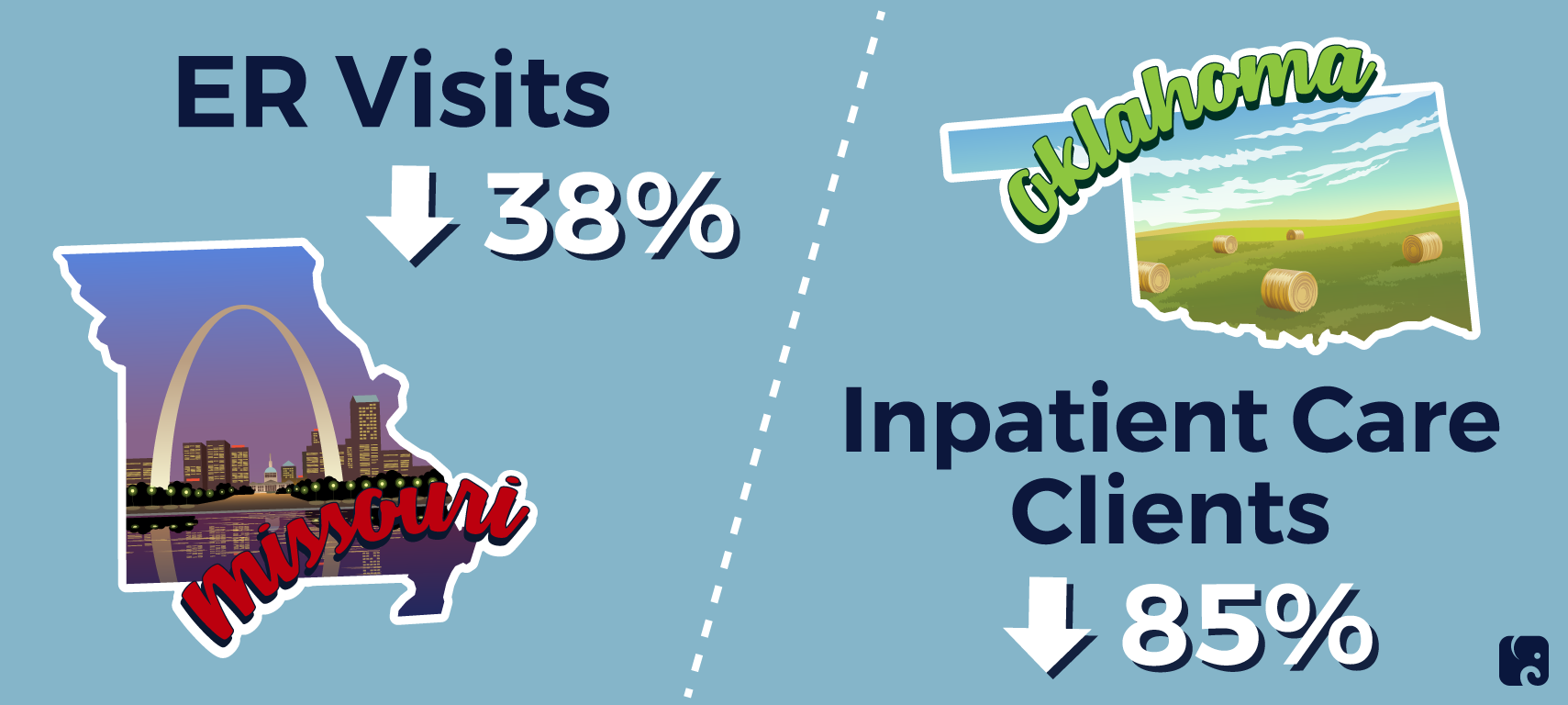
The early results are encouraging. In Missouri, the clinics have reduced hospital encounters by 23% and emergency room encounters by 38% since the beginning of the program. Between 2017 and 2019, more than 38,000 patients were referred by law enforcement to a CCBHC in Missouri. This has reduced the burden on the criminal justice system by giving officers better alternatives – rather than the ER or jail – for helping people who are experiencing a mental health crisis. One facility in Oklahoma reported that since joining the program it has served 6,644 “crisis stabilization clients” – people having a psychiatric emergency. It says 85% of them were diverted from inpatient care, saving taxpayers $56.5 million.
Next Article Previous Article
